
Artificial Intelligence for Healthcare Payer Market Size, Share, Trends, Industry Analysis Report
By Component, By Deployment, By Technology, By Application, and By Region – Market Forecast, 2025–2034
- Published Date:Oct-2025
- Pages: 122
- Format: PDF
- Report ID: PM6485
- Base Year: 2024
- Historical Data: 2020-2023
What is the artificial intelligence for healthcare payer market size?
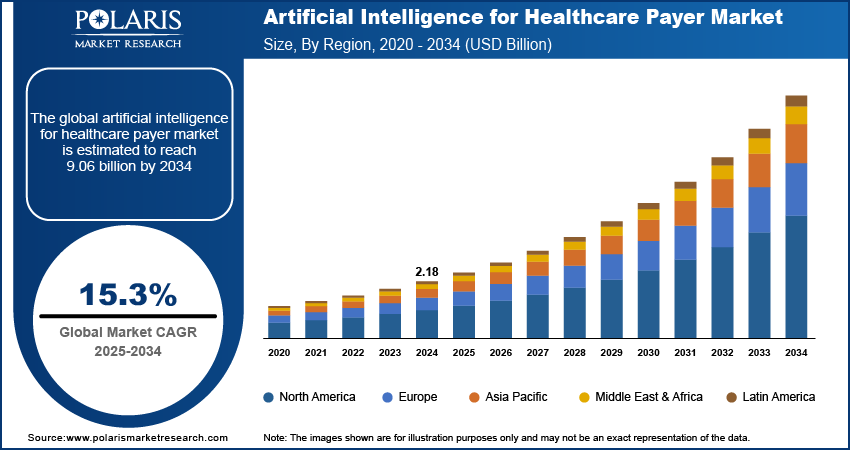
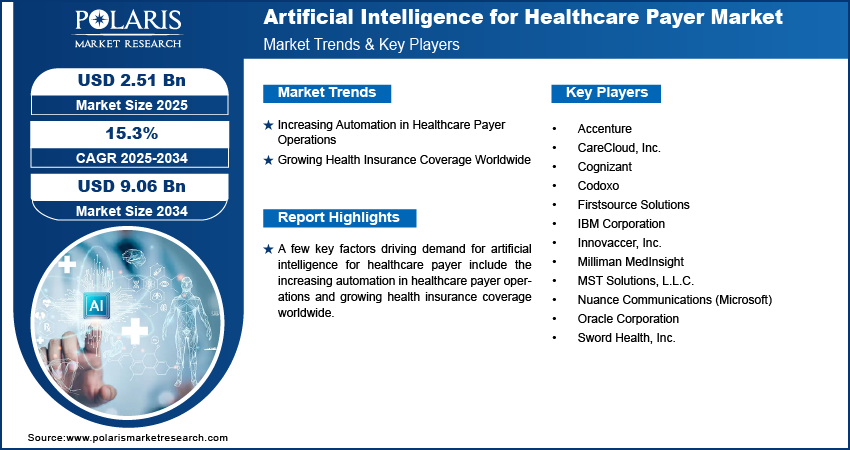
The global artificial intelligence for healthcare payer market size was valued at USD 2.18 billion in 2024, growing at a CAGR of 15.3% from 2025 to 2034. Key factors driving demand for artificial intelligence for healthcare payer include the increasing automation in healthcare payer operations and growing health insurance coverage worldwide.
Key Insights
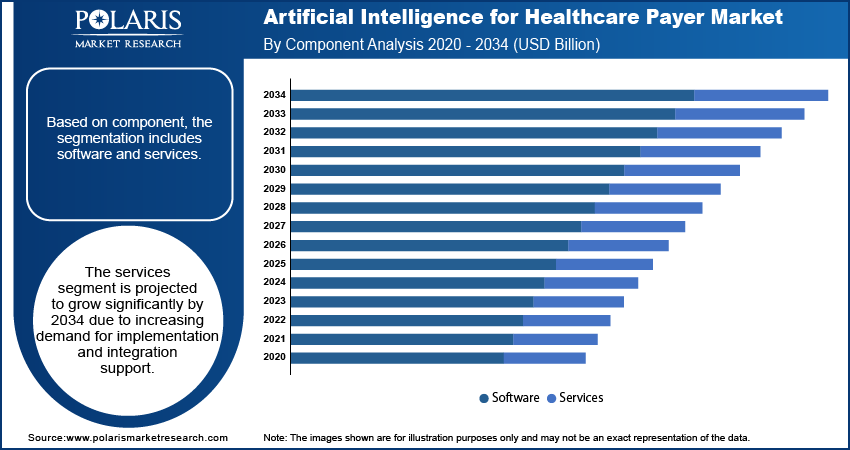
- The software segment dominated the market share in 2024.
- The services is expected to grow rapidly due to rising demand for AI implementation, integration, and managed support.
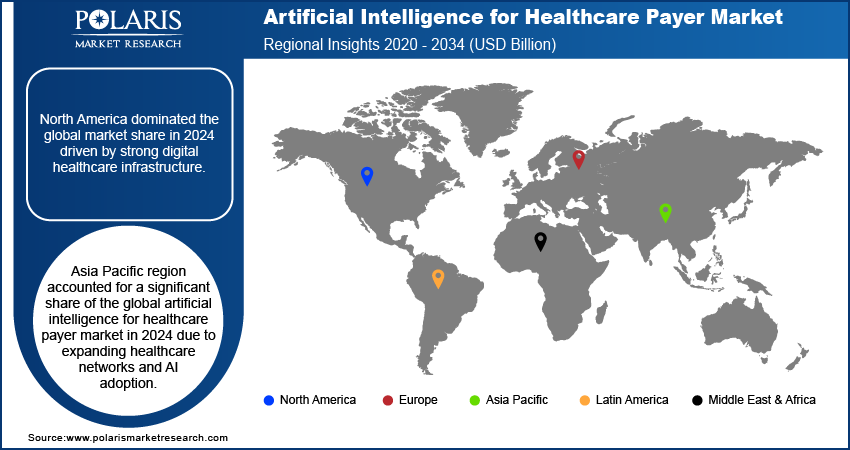
- North America artificial intelligence for healthcare payer market dominated the global market share in 2024.
- The U.S. artificial intelligence for healthcare payer market is growing due to high digitalization in payer operations and robust healthcare spending.
- The market in Asia Pacific is projected to grow at a fast pace from 2025-2034, propelled by rapid adoption of AI technologies.
- China and Japan drive regional growth with expanding insurance networks and investments in digital health solutions.
Industry Dynamics
- Increasing automation in healthcare payer operations is boosting market growth by reducing costs and improving efficiency.
- Growing health insurance coverage worldwide is driving demand due to higher need for claims management and fraud detection.
- The integration with telemedicine platforms is expected to create lucrative opportunities during the forecast period.
- Data privacy and regulatory compliance challenges is anticipated to restrain market growth.
Market Statistics
- 2024 Market Size: USD 2.18 Billion
- 2034 Projected Market Size: USD 9.06 Billion
- CAGR (2025–2034): 15.3%
- North America: Largest Market Share
What is artificial intelligence for healthcare payer market?
Artificial intelligence for healthcare payer utilizes data analytics and machine learning to improve insurance and administrative procedures. It supports claims automation, fraud detection, risk assessment, and policy management with higher accuracy. These tools allow payers to reduce costs, enhance service quality, and make faster decisions. Growing digital adoption and data expansion are driving the use of AI in healthcare payer worldwide.
Rising government healthcare spending is boosting the AI for healthcare payer market through investments in claim management systems and patient care improvement. As per the World Health Organization, overall world health expenditure stood at about USD 9 trillion in 2021. In addition, government expenditure in 2023 on health accounted for 10.1% of German GDP and 9.5% of that of Japan, driving demand for AI-based solutions.
Growing cases of false claims and billing errors are driving the AI for healthcare payers market where payers employ AI to identify anomalies and automate claim validation. The urge to reduce financial losses and inefficiencies is pushing its adoption across the world.
Drivers & Opportunities
Which are the factors driving artificial intelligence for healthcare payer market growth?
Growing Automation in Healthcare Payer Operations: The AI for healthcare payer market is growing with increasing automation in payer operations that reduces costs, decreases claim denials, and enhances coordination between payers and providers. For instance, Oracle recently released AI-based applications to automate prior authorizations and streamline value-based care programs, boosting the adoption of AI to simplify healthcare payer operations.
Growing Health Insurance Coverage Worldwide: Increasing health insurance coverage is propelling the artificial intelligence for healthcare payers market with the increasing number of insured patients. This increases the number of claims and administrative complexity, which encourages payers to implement AI solutions to manage claims in a streamlined manner, cost containment, and improved patient care coordination.
Segmental Insights
Component Analysis
By component, the market is divided into software and services. The software segment led the market in 2024 due to its increasing application in claims automation, better fraud detection, and improved operational efficiency. Integration with predictive analytics and cloud systems boosts its position among major healthcare payers.
The services segment is expected to grow the fastest as payers look to AI system installation, integration, and data management for assistance. Increasing demand for tailored solutions, compliance administration, and technical support is driving this segment's growth.
Deployment Analysis
By deployment, the market is divided into cloud and on-premises. The cloud segment led in 2024 due to its scalability, flexibility, and capacity to handle real-time data in large networks. It minimizes infrastructure costs and maximizes the convenience of data access for healthcare payers.
The on-premises segment is expected to develop steadily as payers prioritize closer data control and compliance. It offers better customization and security in handling sensitive claims and patient information making it suitable for larger organizations.
Technology Analysis
By technology, the market includes machine learning (ML), natural language processing (NLP), predictive analytics, and others. The ML segment dominated in 2024 as it helps in automating claims, identifying fraud and enhances the accuracy of cost prediction. Its capability to learn from massive datasets ensures more efficient and accurate decisions for payers.
The NLP segment is set to grow the fastest due to its application in processing unstructured data from patient records and claims. It enhances documentation accuracy, automates communication, and raises member satisfaction.
Application Analysis
By application, the market includes claims processing optimization, fraud detection and prevention, revenue management and billing, administrative workflow automation, and others. The claims processing optimization segment dominated the market in 2024 as AI improves claim accuracy, reduced costs, and shortenes approval times. In February 2025, VoiceCare AI partnered with Mayo Clinic to test a voice AI system that automates healthcare calls and simplifies benefit verification, authorizations, and claim processing.
The fraud detection and prevention market is anticipated to expand the most with growing cases of fraud and the need for better financial protection. Systems based on AI detect suspicious activity in real-time and minimize false alarms enhancing payer confidence and compliance.
Regional Analysis
North America led the AI for healthcare payers market in 2024 due to its extensive use by payers in managing claims, risk assessment, as well as detecting fraud. Strong healthcare infrastructure, high digitalization, and government initiatives for value-based care are accelerating AI adoption across insurance providers.
The U.S. Artificial Intelligence for Healthcare Payer Market Insights
Rising healthcare expenditure in the U.S. is driving growth in the AI for healthcare payers market through increasing investment in AI-driven claims management and fraud detection. The Centers for Medicare & Medicaid Services estimated that U.S. health spending hit about USD 4.9 trillion in 2023, up from USD 4.1 trillion in 2020. This growth is opening up greater access to advanced AI tools for greater operational efficiency and overall improved payer-provider coordination.
Europe Artificial Intelligence for Healthcare Market Assessments
The Europe market is expected to account for a significant revenue share in 2034 driven by mature healthcare systems, stringent rules, and investments in AI platforms for claim handling and predictive modeling. EU digital health programs and reimbursement policies are also urging AI implementation in payer functions.
Asia Pacific Artificial Intelligence for Healthcare Payer Market Trends
Asia Pacific is expected to grow fastest driven by increasing healthcare expenditures and private insurance growth that enhance administrative effectiveness. Investments in digital health platforms, telehealth expansion and government digitization initiatives are driving AI adoption among payers.
India Artificial Intelligence for Healthcare Payer Market Overview
The increasing demand for customized health insurance options is contributing to growth in the AI for healthcare payers market as it helps in efficient policy choice, precise coverage determination and increasing customer interaction. For instance, Future Generali India introduced in April 2025 an AI-enabled platform that simplifies and personalizes the selection of the correct health insurance coverage for a person enabling quicker, better and more personalized policy selection.
Key Players & Competitive Analysis
The market for healthcare payers is extremely competitive, with major players including Nuance Communications (Microsoft), IBM Corporation, Oracle Corporation, Accenture and Cognizant. These firms develop AI products for claims handling, fraud detection, risk assessment, and personalized care to improve the payers' efficiency and reduce their expenses. Competition also arises from collaboration and launches to extend AI capabilities and accelerate deployment of solutions.
Who are the major players in artificial intelligence for healthcare payer market?
A few major companies operating in the artificial intelligence for healthcare payer industry include Nuance Communications (Microsoft), IBM Corporation, Oracle Corporation, Accenture, Cognizant, Milliman MedInsight, Firstsource Solutions, Sword Health, Inc., CareCloud, Inc., MST Solutions, L.L.C., Innovaccer, Inc., and Codoxo.
Key Players
- Accenture
- CareCloud, Inc.
- Cognizant
- Codoxo
- Firstsource Solutions
- IBM Corporation
- Innovaccer, Inc.
- Milliman MedInsight
- MST Solutions, L.L.C.
- Nuance Communications (Microsoft)
- Oracle Corporation
- Sword Health, Inc.
Artificial Intelligence for Healthcare Payer Industry Developments
September 2025: Milliman MedInsight launched the MedInsight Innovation Portal, a next-generation, AI-powered cloud analytics platform designed to empower healthcare organizations. It offers payers with advanced AI capabilities, seamless data integration, and automated analytics to improve decision-making and operational efficiency.
August 2025: Firstsource Solutions partnered with Guidehealth to speed up value-based care powered by AI for health plans. The partnership is designed to enhance models of care, maximize claims handling, and grow member participation, resulting in better health outcomes and operating effectiveness.
July 2025: Sword Health launched Sword Intelligence with AI-powered care manager agents designed to help payers, providers, and governments fight healthcare's operational problems.
Artificial Intelligence for Healthcare Payer Market Segmentation
By Component Outlook (Revenue, USD Billion, 2020–2034)
- Software
- Services
By Deployment Outlook (Revenue, USD Billion, 2020–2034)
- Cloud
- On-Premises
By Technology (Revenue, USD Billion, 2020–2034)
- Machine Learning (ML)
- Natural Language Processing (NLP)
- Predictive Analytics
- Others
By Application Outlook (Revenue, USD Billion, 2020–2034)
- Claims Processing Optimization
- Fraud Detection and Prevention
- Revenue Management and Billing
- Administrative Workflow Automation
- Others
By Regional Outlook (Revenue, USD Billion, 2020–2034)
- North America
- U.S.
- Canada
- Europe
- Germany
- France
- UK
- Italy
- Spain
- Netherlands
- Russia
- Rest of Europe
- Asia Pacific
- China
- Japan
- India
- Malaysia
- South Korea
- Indonesia
- Australia
- Vietnam
- Rest of Asia Pacific
- Middle East & Africa
- Saudi Arabia
- UAE
- Israel
- South Africa
- Rest of Middle East & Africa
- Latin America
- Mexico
- Brazil
- Argentina
- Rest of Latin America
Artificial Intelligence for Healthcare Payer Market Report Scope
|
Report Attributes |
Details |
|
Market Size in 2024 |
USD 2.18 Billion |
|
Market Size in 2025 |
USD 2.51 Billion |
|
Revenue Forecast by 2034 |
USD 9.06 Billion |
|
CAGR |
15.3% from 2025 to 2034 |
|
Base Year |
2024 |
|
Historical Data |
2020–2023 |
|
Forecast Period |
2025–2034 |
|
Quantitative Units |
Revenue in USD Billion and CAGR from 2025 to 2034 |
|
Report Coverage |
Revenue Forecast, Competitive Landscape, Growth Factors, and Industry Trends |
|
Segments Covered |
|
|
Regional Scope |
|
|
Competitive Landscape |
|
|
Report Format |
|
|
Customization |
Report customization as per your requirements with respect to countries, regions, and segmentation. |
FAQ's
The global market size was valued at USD 2.18 billion in 2024 and is projected to grow to USD 9.06 billion by 2034.
The global market is projected to register a CAGR of 15.3% during the forecast period.
North America dominated the market in 2024 driven by early adoption of AI and advanced analytics in payer operations.
A few of the key players in the market are Nuance Communications (Microsoft), IBM Corporation, Oracle Corporation, Accenture, Cognizant, Milliman MedInsight, Firstsource Solutions, Sword Health, Inc., CareCloud, Inc., MST Solutions, L.L.C., Innovaccer, Inc., and Codoxo.
The cloud segment dominated the market revenue share in 2024 due to scalability, flexibility, and faster deployment.
The fraud detection and prevention segment is projected to witness the fastest growth during the forecast period due to rising healthcare fraud cases.
